Yasmine Khan
Service Designer
Northstar Service Design
Challenge: A clinic in crisis
When the pandemic hit the organization rolled out telemedicine services in just 6 weeks in order to retain customers. Clinical and para-clinical operations were chaotic. Backstage, clinicians and support staff used several instances of Salesforce + 3 different EHRs. Staff & customers raised concerns about the quality of patient care under these conditions.
An upcoming merger applied pressure to create a longterm service vision that could scale.
My role was to learn the landscape deeply. Simplify its complexity to facilitate customer & staff centric decision making. And create solutions that cross functional stakeholders could align and deliver on.
Expertise provided
Service audit & user research.
Creating a service blueprint that makes sense of complex dependencies.
Creating a human centered design strategy to solve the problems identified.
Executing and leading design on a v1 Northstar prototype.
Planning an evolution toward Northstar that addresses the needs of clinical staff, the business, and engineering.
Delivered in 3 months
Clear stories about what service delivery looks like end to end. As well as a detailed service blueprint to objectively track dependencies and the root cause of issues.
Product strategy & a user-validated northstar prototype that gave us something meaningful and realistic to work toward.
Service blueprint
Top Row - Front stage. Direct touchpoints with patients. (Insurance card. Phone. Nurse. Email. Website, etc.)
Second Row - Backstage. Staff interactions & hand offs.
Third Row - Internal digital systems.
Fourth Row - External digital systems.
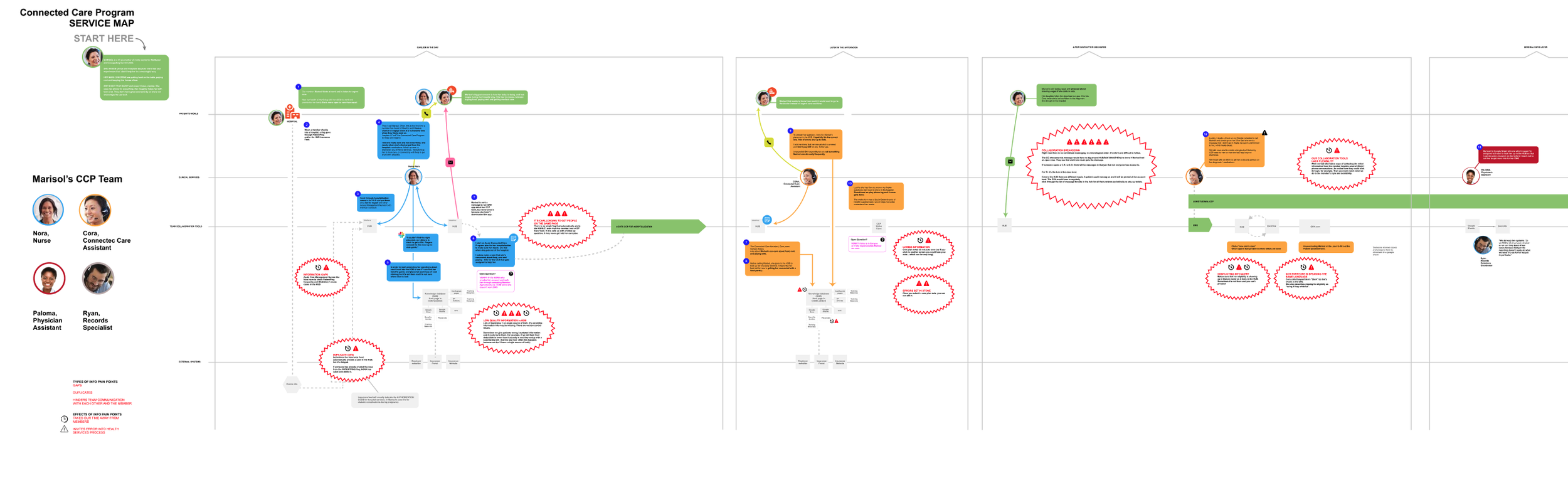
What made the blueprint matter
-
Making it clear that “squeaky wheel” staff are not simply overworked disgruntled employees. Contradictions and gaps in information at every step of service delivery are clearly laid out. When it’s mentionable its manageable!
-
The audit allowed us to start extrapolating on the $ cost of excessive toil like redundant data entry. Back-of-the-napkin early estimates were at $2M per year.
In this clearer landscape, we were also ready to establish patient and staff satisfaction metrics. In order to continue to monitor the toll on quality that broken systems take. -
Now that we’ve made sense of service delivery touchpoints - and datapoints - on an individual level, we’re prepared to do meaningful reporting on a population level.
Reporting informs staffing decisions, performance reviews, product prioritization and service offerings.
Tanya Parr, Physician’s Assistant
“We as clinicians spend so much time on so many different systems and platforms. It's truly mentally exhausting for us and it's not safe for members (patients). ”
insights -> strategy
Insights
-
Patient care includes wrap around services like insurance navigation and getting expert opinions. Not everyone can access all systems. So staff must redundantly document data, which creates room for error.
Clinicians spend ~20 min on redundant documentation for routine patient encounter.
Non-clinical staff spend ~10 minutes on redundant documentation to for routine patient encounters. (ie: I left a voicemail)
No one gets clarity about what’s going on with any given patient.
-
Clinical & Care Staff regularly encounter members..
.. with financial obstacles to medicine and care
.. with terminal diagnosis
.. with sick or dying children
.. struggling with self harm or substance abuse
Each staff member uses 3-6 systems at a time while responding to these sensitive needs.
Patient data can differ from system to system. There is no source of truth.
Bouncing between tools with unique architectures is disorientating.
Terminology also differs from system to system.
Together these factors are a recipe for disaster. Every clinician and staff member I spoke to had stories about slip ups and misses that hurt patients and embarrassed them as professionals.
-
It’s impossible to confidently track what’s going on for an individual patient. Let alone track what’s happening at population level.
Being in the dark about patients invites career risk for clinicians. Health risk for patients. Financial risk for the business. Altogether, hurting team morale and the business.
Prioritization feels like guesswork for product, engineering & operations leadership.
Northstar Strategy
-
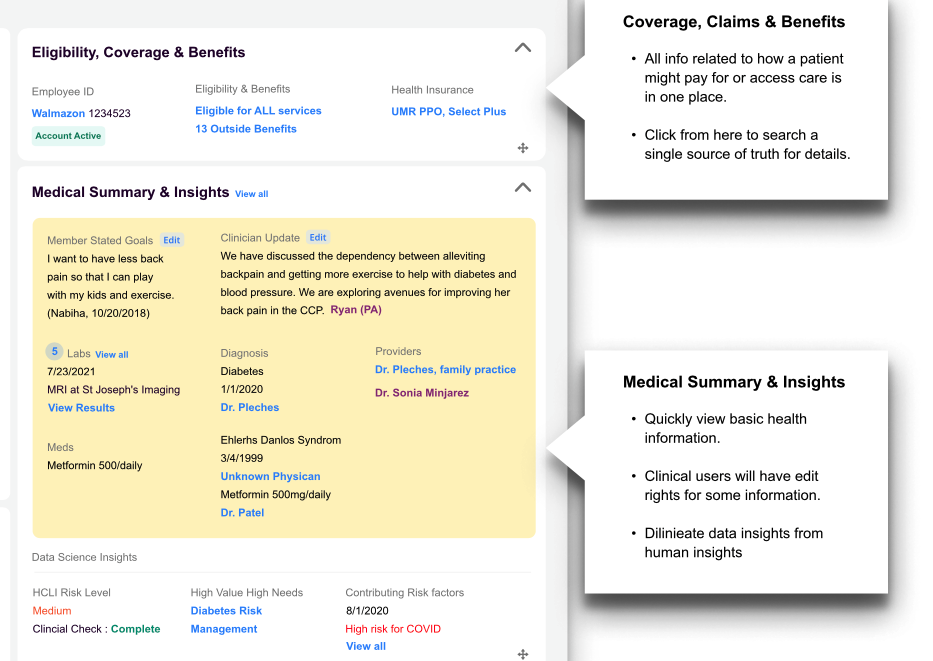
Eliminate redundant data entry.
Provide a snapshot view of patient info.
Make it easy to see who’s working on what with the patient. And what the next steps are.
Provide a timeline of care that includes internal and external services.
Capture social information that impacts service delivery. (ie: parental custody agreements, need for LGBTQIA supportive care, financial barriers to care, etc.)
Offer insurance coverage information that’s easy enough for clinicians to understand, and detailed enough for service staff to use.
-
Side by side view of different types of information.
Bring the most relevant details forward.
Make it something you can look at all day without getting fatigued sorting through noise.
-
Offer a way for operations to track the volume, efficiency and quality of each service type. To inform product, engineering prioritization. As well as operations decisions, like staffing needs performance evaluations.
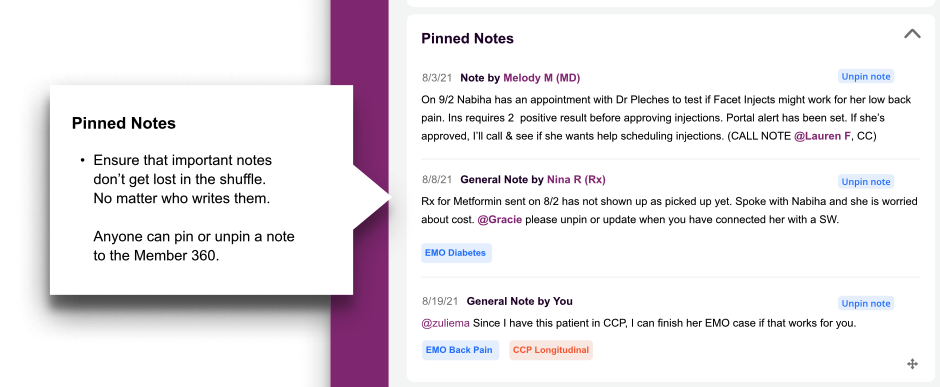
v1 Northstar Prototype
dashboard for all
zoom in
What Users Said
“I would probably get back 5-10 hours a week if everything was housed in one system like this. ”
— Ana Robles, Connected Care Assistant
“With a tool like this, I could complete twice as many cases in a week, if not three times as many. Please find a better way for clinicians and staff to access and share information like this. The fragmented systems bury information so deeply it’s like going on a scavenger hunt to answer a question. It’s a patient safety and satisfaction issue.”
— Tara Parr, Physicians Assistant
“I would get back 10 hours a week with this. All the bouncing around we do today adds up to make comprehensive medication reviews take two hours.”
— Nina Kleinschmidt , Pharmacist
Evolving toward northstar
COMING SOON: How we plan to evolve from current state to the northstar. Addressing the needs of
clinical staff, patients & customers
the business
engineering